Managing diabetes can be tricky, and despite your best efforts to incorporate healthy lifestyle changes, additional support may be needed to get your blood sugar readings down. Enter medications! Medications can be seen as tools that help fine-tune areas where the body may be having challenges. You and your doctor will decide what works best for you. Let’s decode each medication according to their action in the body.
To keep things simple, we’ll refer to each medication by its drug class and brand name first, with the generic name in parentheses. For example, biguanides are the drug class, and metformin (Glucophage) is the generic name. This approach helps you understand how each medication works and makes it easier to recognize, even if it’s sold under different brand names. Keep in mind: medications within the same class often work in similar ways, may have similar benefits, and are used to treat the same condition.
Disclaimer: People with Type 1 diabetes always need insulin, though other medications may sometimes be added to help with blood sugar control. For Type 2 diabetes, treatment can include pills, injections, or a mix of both—depending on your individual needs. The medications mentioned in this article are commonly used for Type 2 diabetes and do not cover every option available. For further medication guidance, see Scheiner (2020) and the American Diabetes Association's website, a widely used resource for diabetes self-management.
Medications by Action
Tells Your Liver to Chill on Making Sugar
Metformin, a biguanide, is a first-line medication for type 2 diabetes. It reduces the amount of stored sugar released by the liver, which often explains why people wake up with high blood sugar. The liver releases sugar during long stints without food, such as overnight or between meals. Good news: metformin is widely prescribed, affordable, generally safe, and has added benefits like improving insulin sensitivity. While some worry it harms kidneys, doctors only adjust or stop it if kidney function is a concern. Interestingly, metformin comes from the French lilac plant (Galega officinalis), used for centuries for diabetes-like symptoms (Bailey, 2004).
Boosts Your Insulin-Making Power
Sulfonylureas (Glimepiride, Glipizide) and meglitinides (Repaglinide, Nateglinide) stimulate the pancreas to produce more insulin—the hormone that unlocks cells so sugar can be used for energy. Sulfonylureas last 12–24 hours, while meglitinides act for 4–6 hours and are taken before meals. Both can cause low blood sugar and weight gain. They are affordable and effective options.
Supports Blood Sugar Control by Flushing Out Excess Sugar
SGLT2 inhibitors help the body expel sugar through urine rather than reabsorbing it. Examples include Invokana (Canagliflozin), Farxiga (Dapagliflozin), and Jardiance (Empagliflozin). They may also support weight loss and protect heart and kidney health. Downsides include higher cost and the need for good hydration.
Turns Up Helpful Gut Hormones
- DPP-4 inhibitors block an enzyme that breaks down GLP-1, a hormone that slows stomach emptying and boosts insulin release. Examples: Januvia (Sitagliptin), Tradjenta (Linagliptin), Nesina (Alogliptin). They’re weight-neutral but expensive.
- GLP-1 receptor agonists and dual GIP/GLP-1 medications mimic gut hormones, lowering liver sugar, slowing digestion, curbing appetite, and increasing insulin. Examples: Ozempic (Semaglutide), Mounjaro (Tirzepatide), Trulicity (Dulaglutide). They often aid weight loss and improve blood sugar but vary in cost.
Helps Insulin Do Its Job
Thiazolidinediones (TZDs) improve insulin sensitivity in muscle and fat cells, helping them use sugar for energy. Examples: Actos (Pioglitazone), Avandia (Rosiglitazone). Affordable but not suitable for people with heart failure or bladder cancer history. May cause weight gain.
Helps Your Body Absorb Carbs More Slowly
Alpha-glucosidase inhibitors delay carb absorption in the small intestine, preventing blood sugar spikes after carb-heavy meals. Examples: Prandase (Acarbose), Glyset (Miglitol). They’re affordable but may cause gas, bloating, or diarrhea.
Stepping In When Your Pancreas Needs Backup
Insulin is a hormone the body produces to regulate blood sugar and metabolism. As mentioned previously, all Type 1 DM patients require insulin and patients with type 2 DM may also need it as an add-on therapy. There are a variety of forms, like long-acting insulin, fast acting-insulin, and mixed insulins that can be delivered in different forms – syringes, pens, patches, and nasal inhalers. Check out our article here for more information on the different types of insulin and how they work.
One Medication, Multiple Benefits
Combination pills can simplify treatment. For example, Janumet combines sitagliptin and metformin; Trijardy combines empagliflozin, linagliptin, and metformin. Ask your doctor if combination therapy is right for you.
Breaking It Down
A chart is included here with common diabetes medications, their action, effect on weight, affordability, and lifestyle habits that can mimic their action. Remember that not everyone will experience weight changes with these medications.
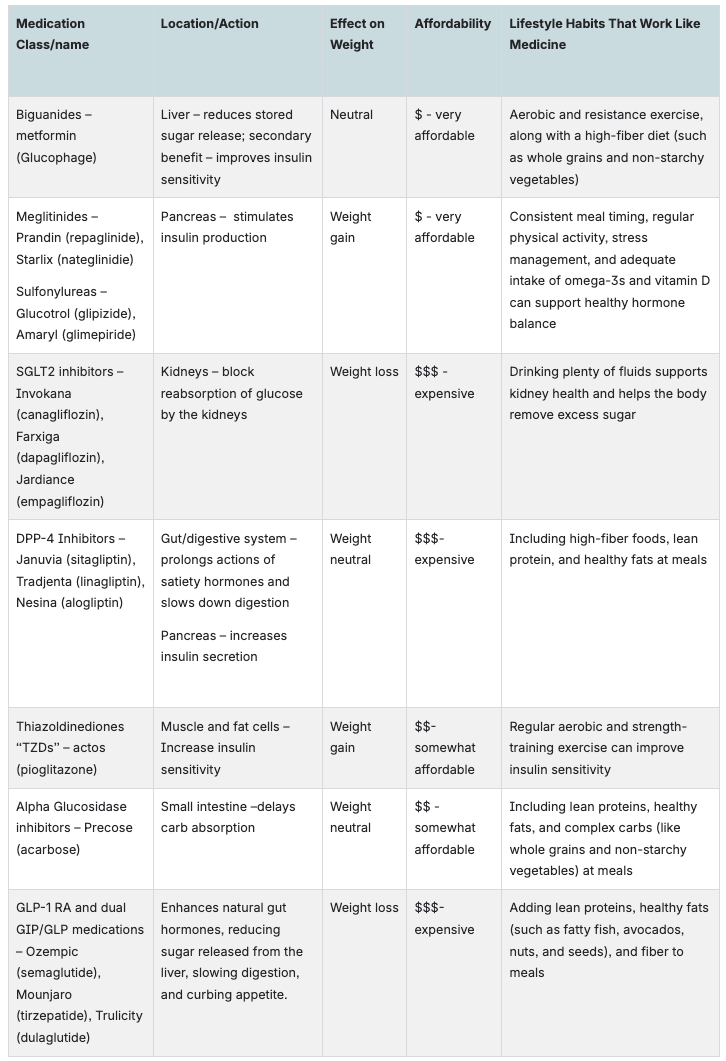
Note: Adapted from *Standards of care in diabetes—2025*, by American Diabetes Association, 2024, *Diabetes Care*, 48(Suppl. 1), p. S181. https://doi.org/10.2337/dc25-S009
Takeaways
- Diabetes medications help manage blood sugar when lifestyle changes aren’t enough.
- They work in different ways: reducing liver sugar, boosting insulin, expelling sugar in urine, enhancing gut hormones, increasing insulin sensitivity, or slowing carb absorption.
- Insulin is essential for Type 1 diabetes and often needed for Type 2.
- Medications can also support weight management, heart health, or kidney health, though cost and side effects vary.
- Lifestyle changes can reinforce the benefits of medication.
References
- American Diabetes Association. (2024). 9. Pharmacologic approaches to glycemic treatment. In Standards of care in diabetes—2025 (Diabetes Care, 48[Suppl. 1], S181–S206). https://doi.org/10.2337/dc25-S009
- Bailey, C. J. (2004). Metformin: Its botanical background. Practical Diabetes International, 21(3), 115–117. https://doi.org/10.1002/pdi.606
- Scheiner, G. (2020). Think like a pancreas: A practical guide to managing diabetes with insulin (3rd ed., Ch. 3). Da Capo Lifelong Books.



